Ketamine is, in fact, used on a daily basis in hospitals around the world. It’s an essential anesthetic, especially in emergency medicine and pediatric surgeries, thanks to its safety profile and its ability to maintain airway reflexes (Sinner & Graf, 2020). Ketamine infusions are also becoming a go-to treatment for individuals battling treatment-resistant depression and acute suicidal thoughts (Zarate et al., 2019).
Myths About Ketamine 3: The Same Dosing is Used for Everyone
Fact: Ketamine dosing is far from one-size-fits-all. Factors like body weight, metabolism, and the condition being treated all play a role. For anaesthesia, a typical intravenous dose ranges from 1-2 mg/kg. However, for psychiatric treatments, much lower doses are used—around 0.5 mg/kg over 40 minutes for depression (Sanacora et al., 2017).
Myths About Ketamine 4: All Forms of Administration Work the Same Way
Fact: The way ketamine is administered matters. Different methods of administration—like intravenous (IV), intranasal, intramuscular, and oral—result in different levels of absorption. IV administration gives near 100% bioavailability, while other forms, like the FDA-approved esketamine nasal spray for depression (Spravato), have a bioavailability of about 48% (Daly et al., 2018). So, not all forms are equal in how they affect the body (Morgan et al., 2018).
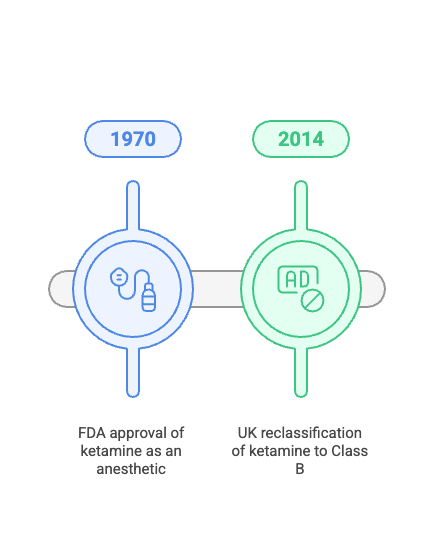
Myths About Ketamine 5: It’s a Brand New Psychiatric Drug
Fact: While ketamine’s use in psychiatry is a hot topic these days, it’s far from a new drug. Originally synthesised in 1962 (Domino, 2010), its antidepressant effects were first noted in the early 2000s (Berman et al., 2000). Over the years, studies have shown ketamine’s rapid-acting benefits for depression (Wilkinson et al., 2017), making it a promising tool in treating mental health conditions.
Myths About Ketamine 6: It’s Only Used in Animals
Fact: Ketamine is well known in the veterinary world, but it’s also widely used in human medicine. Though the formulation and dosing might differ between humans and animals, the drug’s dissociative and analgesic properties are leveraged in both settings (Wax et al., 2022).